ChemSex and Hepatitis C: A Guide for Healthcare Providers

This comprehensive package compiled by 56 Dean Street in London, England is directed towards all service providers looking to garner insight into the associations between PnP and hepatitis C (HCV). Although, in this package, the term chemsex is used interchangeably with PnP. Overarchingly, the guide includes a glossary to familiarize service providers with language used amongst men who have sex with men (MSM), as well as key facts surrounding patterns of use and interactions between substances. In addition, the guide follows from the recognition that some MSM may represent the culmination of all three HCV high-risk subgroups, injection drug users (IDU), people living with HIV (PLWH) and men who have sex with men. Accordingly, it is vital that service providers recognize these intersections and their relevance for appropriate prevention and care.
The guide begins by describing the HCV risks MSM experience when participating in chemsex and seeks to improve the confidence and skill of service providers in communicating these risks and regularly testing clients. Moving forward, the guide describes that a major challenge for service provision in the chemsex sector is to encourage patients to disclose certain behaviours that put them at risk; due to the widespread stigmatization of substance use and gay sex, MSM may be hesitant to access mainstream drug services, and there seems to be some discrepancies between what is shared in the context of traditional drug services vs LGBTQ+-specific services.
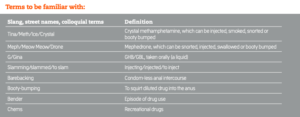
Accordingly, the authors highlight that the use of colloquial terms for drugs/drug use and sex practices by service providers is significant for encouraging honest disclosure. In the next section, the guide puts forth some useful questions to ask during a consultation with a client who PnPs; by toning down pathology and using language that is familiar and absorbable, patients are more likely to retain information days later, and potentially while intoxicated. For instance, asking ‘Do you prefer bareback sex?’ is phrased in a non-judgemental way, meanwhile, ‘Are you comfortable discussing HCV with partners?’ recognizes that having conversations surrounding sexual health can be challenging and may require some additional support. The guide also emphasizes the importance of testing and early treatment for HCV, recommending that service providers include HCV testing alongside regular HIV testing.
Ultimately, this guide is a great starting point for service providers looking to better understand the current situation for PnP. Moreover, this package represents one of the only PnP resources for service providers that includes considerations for HCV within the PnP scene. Accordingly, this resource is undeniably useful for describing the intersections between PnP and HCV, as well as for guiding discussions surrounding HCV in the party scene. Check out the link below to hear Dr. Christopher Whiteley talk more about the intersections of chemsex and HCV and the importance of providing non-stigmatizing and validating treatment environments for MSM.
56 Dean Street. (2014, December). ChemSex and hepatitis C: a guide for healthcare providers. 56 Dean Street. http://www.hcvaction.org.uk/sites/default/files/resources/ChemSex-Hep-C-Guide.pdf
