ChemSex Care Plan
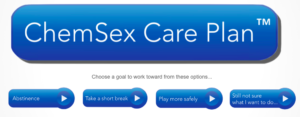
Upon beginning the module, GBMSM are encouraged to choose a goal to work toward: abstinence, take a short break, play more safely, or still unsure of what I want to do. Stuart conceptualizes abstinence as involving adapting to a change-of-life, negotiating sober sex and horny-ness and learning to manage raw emotions and vulnerability without the support of crystal. As well, Stuart emphasizes the significance of the peer-support that can be bolstered from programs such as the Twelve Step, describing this type of support as instrumental for facilitating in community building and mutual understanding. For GBMSM not looking to commit to abstinence, clients can select “take a short break”. Here, GBMSM can specify the time period that they feel would give them a sense of accomplishment or control over their crystal use, ranging from one day to four months.
In addition, clients are prompted to describe how important completing the goal is to them, and how confident they feel in achieving said goal, ranging from one (not important/not confident) to ten (very important/very confident). By relying on this scale, the provider and client can gauge the perceived need for making change – a score below 6 signifies that the goal is not enormously important to the client, suggesting that there isn’t any need to force change upon the client. However, in contrast, if the client scores 7 or higher, signifying that it is important for them to achieve abstinence for a short period of time, the client is directed to complete a questionnaire to identify triggers. This questionnaire also allows a client and their provider to identify the times of the week when they’re most vulnerable to using chems. By outlining triggers and common times/places where the client is triggered, the provider and client can work together to develop a plan to minimize triggers and build relevant support plans.
For GBMSM who are looking to continue playing, but doing so more safely, Stuart overviews “playing more safely”. In this section, Stuart outlines the substances involved in PnP, how they work, and how to use them as safely as possible. Stuart emphasizes that the most commonly experienced harms are STBBIs rather than drug-related harm, providing a solid opportunity for providers to discuss PrEP, PEP, condom use and frequency of HIV and HCV testing. As well, Stuart creates space for discussing the risk of drug-induced psychosis. Together, this section of the plan situates the provider well to engage in discussions surrounding harm reduction and mental health, working with the client to build their toolkit and conceptualize a plan for playing more safely. In comparison, for GBMSM uncertain about what they are looking to do, Stuart provides a questionnaire to consider the pros and cons of using crystal. Here, the client is asked to consider if they miss days at work/university or college because of crystal, and to outline what percentage of their sex lives involve chems, such as crystal or GHB. The client is prompted to reflect on these responses, and make sense of them in consideration of sex, the gay scene and happiness.
Ultimately, Stuart’s ChemSex Care Plan provides a practical platform that service providers could use alongside their clients to best understand their client’s perceptions, use patterns, and risks related to PnP. As well, the platform is highly sex-positive and harm reduction focused, and flawlessly integrates considerations for sex and substance use into a neatly packaged care plan. See below for further details on how to use the care plan in practice.
Stuart, D. (n. d.). ChemSex Care Plan. David Stuart. https://davidstuart-org.webs.com/care-plan
